Views expressed in opinion columns are the author’s own.
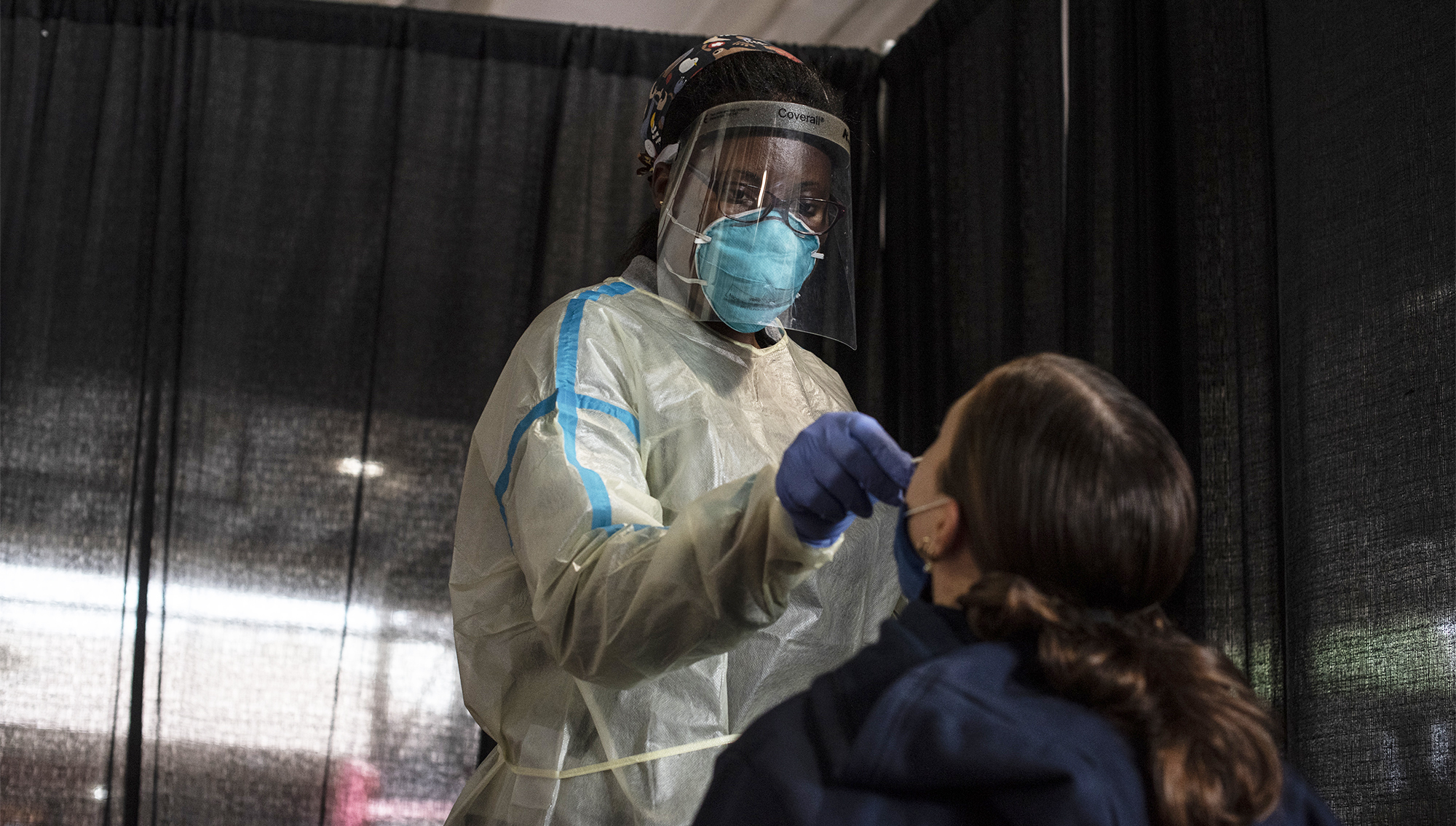
Women face hostile work environments and gender discrimination on a daily basis — and the medical field is no exception. A 2018 report by the National Academies of Sciences, Engineering, and Medicine found that female medical students were 220 percent more likely than students in non-STEM fields to experience sexual harassment. In fact, up to half of female medical students reported being sexually harassed during their training. And among U.S. medical school faculty, 1 in 3 women reported experiencing gender harassment at work in 2019.
These numbers scare me — not just as an aspiring physician, but also as a patient.
STEM fields, including the medical field, are historically male-dominated and, like many institutions in America, entrenched in systemic gender inequality. This has insidious, top-down effects that exacerbate an already stressful environment for women. Gender inequality in medicine doesn’t just hurt female doctors. It also hurts female patients.
While women make up over 50 percent of medical school matriculants, practicing male doctors still outnumber female doctors 64 to 36 percent. And men in the field often occupy positions of power. While men make up the majority of faculty positions at medical schools and dominate the highest-paying specialties, women experience high rates of attrition throughout their medical careers. Almost 40 percent of women physicians go part-time or leave medicine altogether within six years of completing their residencies, citing factors such as work-family conflict, gender harassment, salary inequity and burnout. It should be noted that these factors do not necessarily exist in isolation, but work together in complex ways to sustain one another.
That’s not the only way gender inequality permeates the medical field. Like many other disciplines, medicine was built upon white male perspectives. Recognized medical literature is based on cases experienced by white men, despite the fact that women often experience symptoms differently. And when medical literature is centered around male experiences, women may miss out on important information regarding their own health.
Combine this with a high proportion of male doctors in positions of authority, and the female patient experience is in jeopardy. Male doctors may have a tendency to minimize the pain of women, brushing it off as irrelevant or overdramatic. Patients are already in such a vulnerable environment, potentially facing a fear of pain or judgment. Not only can this hostility make a woman feel uncomfortable at a doctor’s office, it can also discourage her from speaking up next time.
For example, heart attacks in women are often incorrectly diagnosed because their symptoms may be more subtle and atypical, sometimes even appearing without chest pain. Many women aren’t aware their symptoms can present differently from a man’s, causing them to seek help long after damage has already occurred. Sprinkle in an apathetic male doctor who attributes her symptoms (“typical” or not) to stress or menstrual pain, and we get a perfect storm of dangerous patient care.
When men occupy positions of power at the top of the hierarchy, it can be difficult to create change. Medical institutions should implement solutions to target the problem as close to its roots as possible. Affirmative programs that support the recruitment, promotion and retention of women should become the norm in both medical schooling and practice. For instance, mentorship programs designed for women have been met with high satisfaction, as have training programs on implicit biases, bystander effects and microaggressions at medical schools and hospitals.
Female patients suffer from the consequences of systemic gender discrimination just as much as female doctors do. While we’re seeing positive changes at the level of medical school enrollment, there’s clearly something happening to cause so much attrition during and after medical school. Whether it’s gender discrimination, work-family conflict or burnout, one thing is certain — female patients are suffering, too.
Allison Cochrane is a senior biology major. She can be reached at allisonc@umd.edu.