Views expressed in opinion columns are the author’s own.
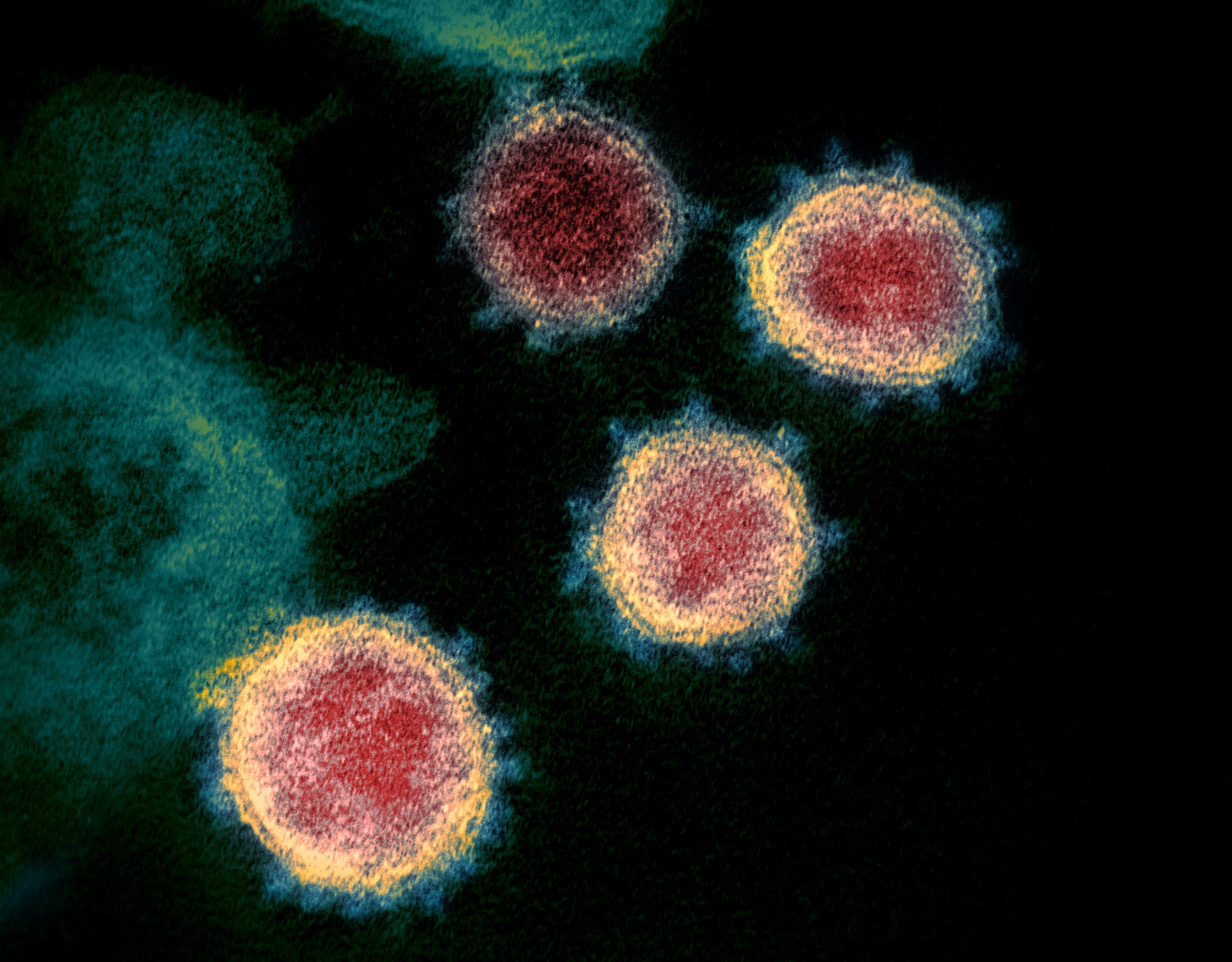
By now, you’re probably well aware of the global shortage of face masks and testing kits that is disrupting efforts to contain the coronavirus pandemic. The situation has become so dire that health care workers have even resorted to reusing protective face masks, jeopardizing their health and greatly increasing their risk of exposure.
However, as the coronavirus continues to peak, we may likely be presented with an even greater dilemma: the ethical rationing of life-saving medical equipment. As difficult as it is to have this discussion, it’s nevertheless important that we establish a rigorous contingency plan in case the situation rapidly deteriorates.
Among various institutions that deal with medical ethics, it appears the consensus is to implement some variation of a utilitarian approach. While the exact criteria may differ depending on a nation’s health care system, the primary objective would be to save as many lives as possible.
Typically, these frameworks assert that all lives are equal, and that wealth, race or any other social construct shouldn’t favor one patient over another. Ironically, there’s a gross contradiction in these guidelines leading to implicit discrimination against the elderly — perpetuating the oft-contentious issue of ageism in medicine.
Before we discuss the potential impact of such an approach, we must understand this framework’s underlying implications. Maximizing lives saved is mutually exclusive with valuing each life equally; such a system implies more robust patients are valued more than their feeble counterparts.
A utilitarian framework examines the consequences of competing actions. If there’s a choice between two patients who require immediate treatment, life-saving equipment would be given to the healthier patient since they’re more likely to survive. If it was instead given to the frailer patient, then the result is less favorable. Not only is that patient more likely to die after being saved, but the healthier patient could’ve survived with the equipment.
The necessary question becomes: How can you reliably determine chances of survival? Given our limited knowledge about COVID-19, do we currently have the resources to reliably predict the future prognoses of afflicted patients? There have been reports of patients being reinfected just days after recovering, as well as patients who initially appear stable but then rapidly deteriorate.
As a result, I think it’s safe to assume that a patient’s current state may not accurately predict their future outcome, especially when compared to another patient in a similar, life-threatening condition. This places a greater emphasis on the patient’s prior health, which is linked to their age. Age is linked with a variety of different health complications and as you become older, you become more susceptible to disease and deteriorating health, which is reflected in the mortality rate of the coronavirus.
While some physicians have avoided this blunt conclusion, others have gone as far to say that, if two patients are in similar conditions but differ in age, then they would provide treatment to the younger patient on the sole basis that they have been “deprived of a full life.”
This interpretation assumes the value of human life is primarily tied to its longevity. Everyone is entitled to a full life — no argument there — but the notion that the experiences we collect along our journey, as well the connections we develop with friends and family, are ultimately secondary compared to the ticking time bomb of our lifespan is a bit unsettling. While a younger patient has more potential, what about the comparatively richer experience base that we’re depriving the elderly patient of? One can argue it seems counterintuitive that human lives somehow become less valuable as we age.
Ultimately, I believe that random chance should play a larger role as the neutral arbitrator involved in these ethical judgments. Ethicists have already recommended a lottery system to settle a “tie” within the same class of patients. However, will we soon have the resources and knowledge to generate meaningful class boundaries? And if we do, are we comfortable with accepting that some lives are more valuable than others? At the end of the day, maybe it’s time we examine our prominent and seemingly unquestioned bias against the elderly.
Kevin Hu is a sophomore physiology and neurobiology major. He can be reached at kevxhu@gmail.com.