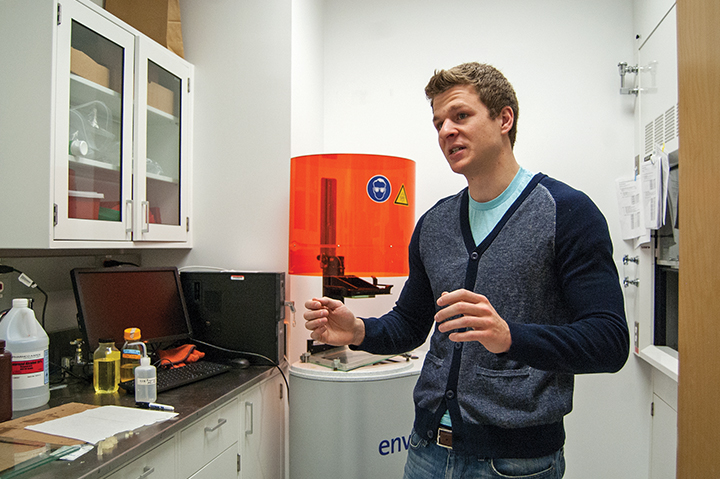
Graduate student Anthony Melchiorri discusses his work with Director John Fisher on 3D-printable vascular grafts.
If all goes according to plan, this university’s bioengineering research could have life-saving applications.
For the past two years, university researchers John Fisher and Anthony Melchiorri have been developing an improved implant method for treating cardiovascular diseases, the leading cause of death globally.
Their technology — patient-personalized 3-D-printed vascular grafts — offers a new take on the already accepted surgical concept of removing a segment of an artery or vein and replacing it with a prosthetic.
The method of 3-D printing is one of the most important and distinguishable features of the new strategy, said Fisher, bioengineering professor and associate chairman.
“We just had a simple idea,” he said. “Instead of making straight cylinders, wouldn’t it be nice if we could make vascular grafts that had an architectural complexity that reflects human anatomy? And in order to do that, we just need to print them.”
Fisher said large-diameter vascular grafts are already available, but they lack the specificity of those he and Melchiorri are constructing. This is a problem, considering the variances in arterial structure from one patient to another, he said.
With the help of a $120,000 3-D printer located in the Kim Engineering Building, Fisher said they can reach precision between 0.05 and
0.1 millimeters, or about one-tenth the thickness of a plastic ID card.
“We’re in the process of trying to print pores in the scaffolds,” he said.
The printer uses a specially designed poly (lactic-co-glycolic acid), or PLGA, to build the grafts. Once implanted, it begins to degrade, encouraging cellular regrowth as it does.
Fisher said the decay time varies, but it would take somewhere in the realm of several weeks to months, a period on the longer side.
“We’ll have to figure out ways to make [the deterioration] faster,” he said.
Melchiorri, a third-year bioengineering graduate student, has spent the past year tweaking the makeup of the material in order for it to work optimally as a 3-D printable vascular graft, he said.
With the technical assistance of Narutoshi Hibino, a microsurgeon at Nationwide Children’s Hospital in Ohio, test mice have received graft implants with successful results so far.
It’s been three months since the surgery, Melchiorri said, and the subjects are alive and well, with good tissue growth observed.
Before pursuing use in human patients, he said the next “shortest long-term goal” is to see similar results in sheep, larger animals with more complicated anatomies.
“We would like to translate this into a clinically applicable technology,” he said. “If everything worked out it’d probably be 15 to 20 years from where we are now.”
The primary obstacle the research is facing is FDA approval, Fisher said. PLGA is not currently approved for use in vascular implants.
It has, however, been approved in other applications like Lupron Depot, an injection treatment for advanced prostate cancer.
But because Fisher and Melchiorri made slight variances to the makeup of the PLGA they use to allow for 3-D printing, this approval would take even more time to go through the FDA.
“If we were to try to commercialize what we’re doing right now, there would be a lot of hurdles in bringing a new material to the market,” Fisher said.